
The ascending aorta lacks its normal curve towards the back and the left of the fetus. The conection between the ductus and the right ventricle (RV) is demonstrated. Bottom left: Similar view to the previous one. It does not connect with the ductus, and bifurcates into the common carotids. The ascending aorta is between the SVC and the ductus.
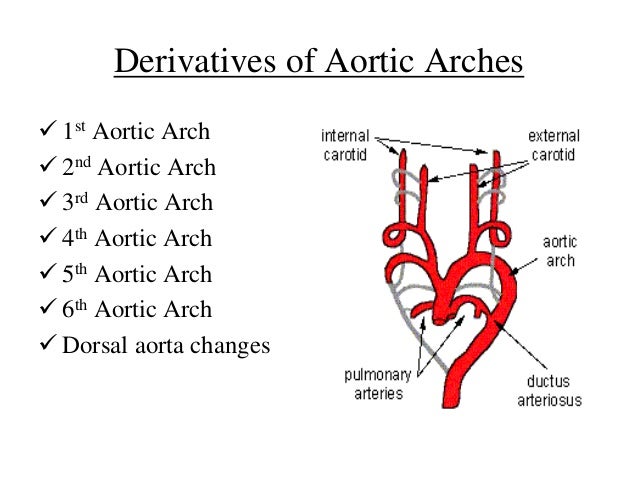
The SVC is seen entering the right atrium (RA). Middle left: This section, just cephalad to the two previous, demonstrates the common carotids and the SVC. Notice the larger size of the ductus compared to the aorta. The relationship between the superior vena cava (SVC), the ascending aorta (asc Ao) and the ductus is seen. 1).įigure 1: Top (left & right): Axial views of the base of the heart. A complex cardiac anomaly was noted (fig. The biometry was consistent with 23 weeks, and an edematous fetus with pleural effusions was found. The examination demonstrated significant polyhydramnios. The diagnosis was confirmed after therapeutic abortion.Ī 42-year-old G 5P 4 patient, whose pregnancy was uncomplicated until the 21 st week of gestation when a discrepancy between size and dates was noted, was referred for a level II scan. Mortality rates for nonimmune hydrops vary from 50 to 95% 1.We report a case of nonimmune hydrops associated with aortic arch interruption in a 23 week fetus with trisomy 21. The underlying pathophysiologic mechanism is related to increased volume and pressure overload of the fetal right atrium, leading to venous hypertension and systemic edema. Nonimmune hydrops has been associated with abnormalities of many organ systems including congenital heart disease and cardiac arrhythmias. MESH Aorta, Thoracic BDE 0050 (when associated with facial palsy and retinal coloboma) ICD9 747.11 CDC 747.215 Delivery should be performed in a tertiary care center with immediate access to a pediatric cardiology service. In the absence of associated anomalies or congestive heart failure, there is no indication to alter standard obstetric management. The option of pregnancy termination should be offered prior to fetal viability, especially in the presence of hydrops. Obstetric management: Careful scanning for associated anomalies and chromosomal studies are recommended. Prognosis: Death usually occurs in the early neonatal period, but survival into childhood has occurred and the lesion has been successfully corrected surgically.ĭiagnosis: In longitudinal view, the ascending aorta follows a straight course to its branches without the normal continuous curvature to the descending aorta.ĭifferential diagnosis: Aortic atresia with hypoplasia of the ascending aorta, aortic coarctation with tubular hypoplasia of the aorta. Multiple other cardiac anomalies are usually present. The aortic valve is bicuspid in nearly half of the autopsied specimens 5. The parietal band of the crista supraventricularis is often absent. The right ventricle is hypertrophied and somewhat dilated, due to the commonly associated VSD. The pulmonary trunk is larger than the ascending aorta, which is often hypoplastic. Pathology: At autopsy the great vessels are usually related in a normal fashon. Pathogenesis: Several mechanisms have been suggested: 1) abnormal involution of the third and fourth aortic arches 6, 2) decreased antegrade bloodflow in the ascending aorta due to the almost constant presence of ventricular septal defects and left ventricular outflow obstructions 11. M1:F1Īssociated anomalies: DiGeorge syndrome (in Type B: 10-50% 6), associated abnormalities of the aortic arch (aberrant or isolated left or right subclavian arteries), intracardiac anomalies (96% 8,9) including VSD, patent ductus arteriosus, left ventricular outflow obstruction (subaortic stenosis or bicuspid aortic valve), truncus arteriosus, CHARGE syndrome (see text).Įtiology: Usually multifactorial but may be associated with aneuploidies and teratogenic exposure (Bis-dichloroacetyl diamene, isotretinoin).

Prevalence: 1:10,000 births,1.3% of children with known heart disease resulting in death, cardiac catheterization, or surgery in the first year of life 2. Each type may be subclassified to indicate association with other cardiac anomalies. 4) A: distal to the left subclavian artery B distal to the left common carotid artery C: distal to the brachiocephalic artery. of Ob-Gyn, Vanderbilt University, 21st & Garland Ave, Nashville, TN 37232-2516 Ph: 61 Fax: 61 andĭefinition: Interruption of the aortic arch between the ascending to descending aorta.Ĭlassification: The classification is based on the position of the interruption relative to the brachiocephalic vessels 3 (fig.


 0 kommentar(er)
0 kommentar(er)
